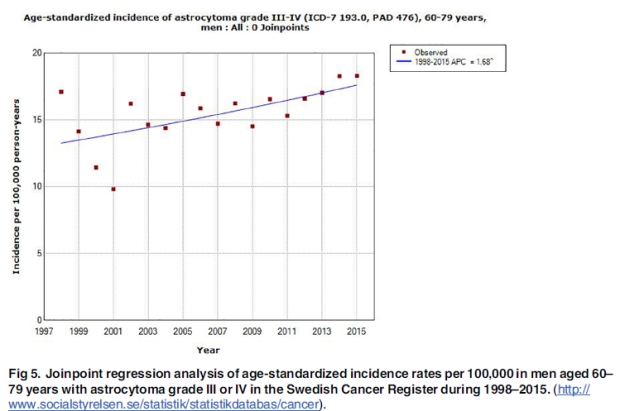
The National Toxicology Program (NTP) animal study on cancer risk from exposure to radiofrequency radiation (RFR) has previously reported an increased incidence of glioma and Schwann cell tumors, that is similar types of tumors as have been reported in human epidemiology. We have commented on the similarity of the findings.
The NTP study presented recently data on DNA damage in the same study, see Smith-Roe SL et al. Evaluation of the genotoxicity of cell phone radiofrequency radiation in male and female rats and mice following subchronic exposure. Environ Mol Mutagen. 2019 Oct 21. doi: 10.1002/em.22343.
Abstract
The National Toxicology Program tested two common radiofrequency radiation (RFR) modulations emitted by cellular telephones in a 2-year rodent cancer bioassay that included interim assessments of additional animals for genotoxicity endpoints. Male and female Hsd:Sprague Dawley SD rats and B6C3F1/N mice were exposed from gestation day 5 or postnatal day 35, respectively, to code division multiple access (CDMA) or global system for mobile (GSM) modulations over 18 h/day, at 10 min intervals, in reverberation chambers at specific absorption rates (SAR) of 1.5, 3, or 6 W/kg (rats, 900 MHz) or 2.5, 5, or 10 W/kg (mice, 1900 MHz). After 19 (rats) or 14 (mice) weeks of exposure, animals were examined for evidence of RFR-associated genotoxicity using two different measures. Using the alkaline (pH > 13) comet assay, DNA damage was assessed in cells from three brain regions, liver cells, and peripheral blood leukocytes; using the micronucleus assay, chromosomal damage was assessed in immature and mature peripheral blood erythrocytes. Results of the comet assay showed significant increases in DNA damage in the frontal cortex of male mice (both modulations), leukocytes of female mice (CDMA only), and hippocampus of male rats (CDMA only). Increases in DNA damage judged to be equivocal were observed in several other tissues of rats and mice. No significant increases in micronucleated red blood cells were observed in rats or mice. In conclusion, these results suggest that exposure to RFR is associated with an increase in DNA damage.
These results add to the evidence that RFR causes cancer. Increased risk is found in both human and animal studies with similarity of tumor types. The new NTP findings add mechanistic effects for carcinogenesis. RFR should be classified as a human carcinogen, Group 1.
Of interest is to compare these NTP exposures with results in the French Phonegate Alert report (https://www.phonegatealert.org/en) on SAR from use of mobile phones. As the table shows with 0 mm distance between the mobile phone and tissue (body contact) SAR values are much exceeding the limits and are actually in the range of those used in the NTP study. These SAR values are to be compared with the manufacture test keeping the phone at some distance from the body. This advice is usually not well informed about to the user but may be found in the instruction manual. This table shows the results presented by Dr Marc Arazi, International Public Symposium, Mainz, Germany, October 6,2019 (with courtesy).
www.phonegatealert.org
SAR comparison : 1gr and 10gr of tissue